We may not have the course you’re looking for. If you enquire or give us a call on 800969236 and speak to our training experts, we may still be able to help with your training requirements.
Training Outcomes Within Your Budget!
We ensure quality, budget-alignment, and timely delivery by our expert instructors.

Psychological Disorders are complex conditions affecting millions globally. These mental disorders, ranging from mild to severe, impact thoughts, feelings, and behaviours, often influencing daily activities and interpersonal relationships.
According to John Hopkins Medicine, approximately 26% of American between the ages of 18 and older has many Psychological Disorders. In an age where Mental Health awareness is gaining momentum, it is important to understand Psychological Disorders. In this blog, you are going to learn what are these Psychological Disorders, why it is important to understand them and some examples of these disorders.
Table of Contents
1) What are Psychological Disorders?
2) The importance of understanding Psychological Disorders
3) Examples of Psychological Disorders
a) Depressive disorders
b) Anxiety disorders
c) Bipolar and related disorders
d) Psychotic disorders
e) Obsessive-compulsive and related disorders
4) Conclusion
What are Psychological Disorders?
Psychological Disorders are disturbances or abnormalities in an individual's cognitive, emotional, or behavioural functioning. They typically arise from a multifaceted blend of genetic, biological, environmental, and Psychological factors. These mental disorders are characterised by persistent patterns that diverge from cultural expectations and can result in significant distress or impairment in daily functioning.
While some individuals with Psychological Disorders might exhibit behaviours deemed as "odd" or "unusual," others might display no overt signs at all. This vast variability makes early detection, understanding, and intervention crucial. The exploration and acknowledgement of these disorders not only facilitate better clinical outcomes but also empower society to move towards a more inclusive and empathetic stance.
Unlock the intricacies of the human mind – Register now in our Psychology Masterclass
The importance of understanding Psychological Disorders
Understanding Psychological Disorders is crucial. Only after understanding them can we get a grasp o f Mental Health. These points will show the importance of understanding Psychological Disorders:

1) Combat stigma: Knowledge about Psychological Disorders eradicates ignorance and challenges societal misconceptions. This helps individuals to seek help without fear of prejudice.
2) Better diagnosis and treatment: A thorough understanding of this mental disorder aids healthcare professionals in accurate diagnosis, staying updated with the latest research, and employing effective therapeutic approaches.
3) Promote inclusive environments: Educators equipped with knowledge can create classrooms where students with disorders are understood and supported, allowing them to reach their full potential.
4) Foster societal empathy: Understanding the challenges faced by those with disorders heightens compassion, leading to more supportive interactions and reduced judgment.
5) Enhance self-awareness: Individuals can recognise early signs within themselves or in loved ones, enabling proactive intervention and support.
6) Resource allocation: With increased acknowledgement of the significance of Mental Health, policymakers are better positioned to allocate resources effectively, ensuring robust Mental Health infrastructures.
7) Public awareness campaigns: Understanding the importance of public health can lead to more impactful public health campaigns, educating the masses and promoting widespread awareness.
8) Community cohesion: A society that understands and respects the nuances of these mental disorders is likely to be more cohesive, with strong support networks for its members.
9) Encourage early intervention: With increased understanding, early detection and interventions become more feasible, often leading to better outcomes for the affected individuals.
Empower your understanding of mental well-being with our course on Mental Health
Examples of Psychological Disorders
To understand fully the various Psychological Disorders, let’s look at some examples:
Depressive disorders
Depressive disorders, also known as depression, encompass a group of conditions which are characterised by continuous feelings of hopelessness, sadness, and a general lack of interest in daily activities. They are among the most common Psychological Disorders globally, affecting millions of people across age groups, genders, and socioeconomic backgrounds.
1) Nature and characteristics of depressive disorders:
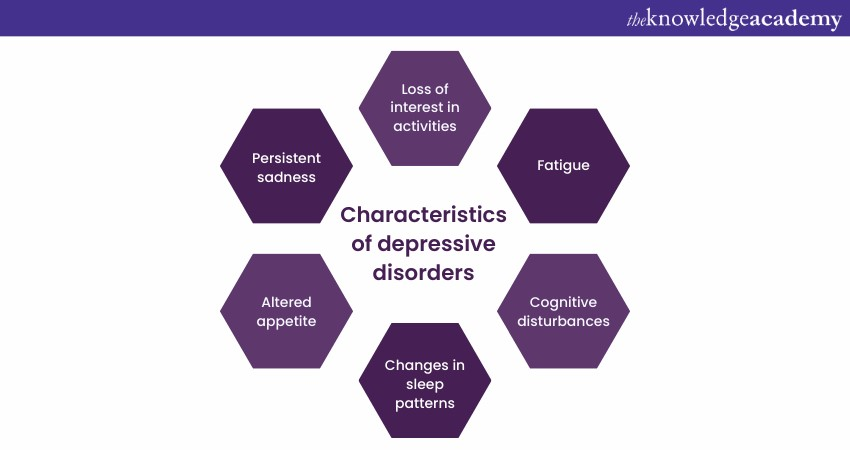
Depressive disorders entail a profound and pervasive sense of despair that can influence almost every facet of an individual’s life. This may include disruptions to sleep patterns, appetite, concentration, and energy levels. People with this type of mental disorder often report feeling empty or numb, and these feelings can lead to a significant decline in daily functioning, sometimes to the point of debilitation.
2) Different Types of depressive Disorders:
a) Major Depressive Disorder (MDD): Often termed 'clinical depression,' MDD is characterised by persistent feelings of sadness and a noticeable disinterest in external stimuli. Individuals must exhibit a cluster of symptoms for at least two weeks to be diagnosed.
b) Persistent Depressive Disorder (PDD): Previously referred to as dysthymia, PDD denotes a chronic form of depression where the symptoms might be milder than MDD but last longer, often extending for years.
c) Bipolar disorder: Although primarily recognised as a mood disorder characterised by manic or hypomanic episodes. Individuals with bipolar disorder frequently experience depressive episodes that are like MDD.
d) Postpartum Depression: A more severe form of the 'baby blues,' postpartum depression affects mothers after childbirth. Hormonal changes, combined with the stresses of caring for a newborn, can lead to this form of depression.
e) Seasonal Affective Disorder (SAD): This is a type of depression which is related to the changes in seasons. SAD generally begins and ends at about the same times every year, usually starting in fall and continuing into the winter months.
3) Causes and risk factors:
The exact cause of depressive Psychological Disorders remains a topic of ongoing research, but they often arise from a combination of factors:
a) Biological: Changes in neurotransmitter levels, particularly serotonin, norepinephrine, and dopamine, have been linked to depression.
b) Genetics: Individuals who have a family history of depression are more likely to experience it themselves.
c) Environmental: Chronic exposure to violence, neglect, abuse, or poverty can make individuals more susceptible to depression.
d) Psychological and personal factors: Personality traits, prolonged stress, trauma, or other mental health disorders can increase the risk.
4) Treatment and management:
a) Psychotherapy: Cognitive-Behavioural Therapy (CBT), Dialectical Behaviour Therapy (DBT), and Interpersonal Therapy (IPT) have been effective in treating depressive disorders.
b) Medication: Antidepressants, which work on neurotransmitters, are commonly prescribed. Selective Serotonin Reuptake Inhibitors (SSRIs) and Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs) are the most prescribed classes.
c) Lifestyle changes: Regular exercise, a balanced diet, adequate sleep, avoiding alcohol and drugs, and stress reduction techniques can be beneficial.
d) Alternative therapies: Electroconvulsive therapy (ECT) and Transcranial Magnetic Stimulation (TMS) are sometimes used for severe cases where other treatments haven't been effective.
Anxiety disorders
Anxiety is a natural emotion, often acting as our body's alarm system, alerting us to potential dangers or concerns. However, for some, this natural response can become overwhelming, frequent, and disproportionate to the actual threat posed by situations. When this heightened state of anxiety becomes chronic and pervasive, affecting one's day-to-day life, it becomes categorised as an anxiety disorder. These points below will help you understand this mental disorder in detail:
1) Types of Anxiety disorders:
There are several specific types, each with its own distinct set of symptoms and triggers:
a) Generalised Anxiety Disorder (GAD): Individuals with GAD experience constant, excessive worry about various aspects of daily life, from health and work to personal relationships and finances. This worry is often unfounded and can be debilitating.
b) Panic disorder: Characterised by recurrent, unexpected panic attacks. These attacks are sudden bouts of intense fear that may include palpitations, sweating, trembling, shortness of breath, and a feeling of impending doom.
c) Social anxiety disorder: This involves an intense fear of being judged, embarrassed, or humiliated in different social situations. It's more than just shyness; it can lead to avoidance of social situations altogether.
d) Specific phobias: This is an extreme fear of a particular object or situation, like fear of heights (acrophobia), spiders (arachnophobia), or flying (aviophobia). Even if the fearful object or situation poses little or no real threat, the person will go to great lengths to avoid it.
e) Agoraphobia: It is a fear of being in situations where escape can be difficult. It also includes fear that help might not be available if things go wrong. Many people assume it's just a fear of open spaces. However, it can also be a fear of being alone, being in crowded places, or travelling on public transportation.
2) Causes of anxiety disorders:
The exact cause of this mental disorder is often complex and multifactorial, involving a combination of:
a) Genetics: A family history of anxiety can increase one's susceptibility.
b) Brain chemistry: Abnormalities in certain neurotransmitters, which are the brain's chemical messengers, can contribute to symptoms.
c) Personality: Certain personality types may be more prone to develop anxiety disorders.
d) Life events: Traumatic events, abuse, or prolonged stress can trigger anxiety disorders in some people.
e) Other medical illnesses: Some medical conditions can trigger symptoms of anxiety or exacerbate them.
3) Symptoms and diagnosis:
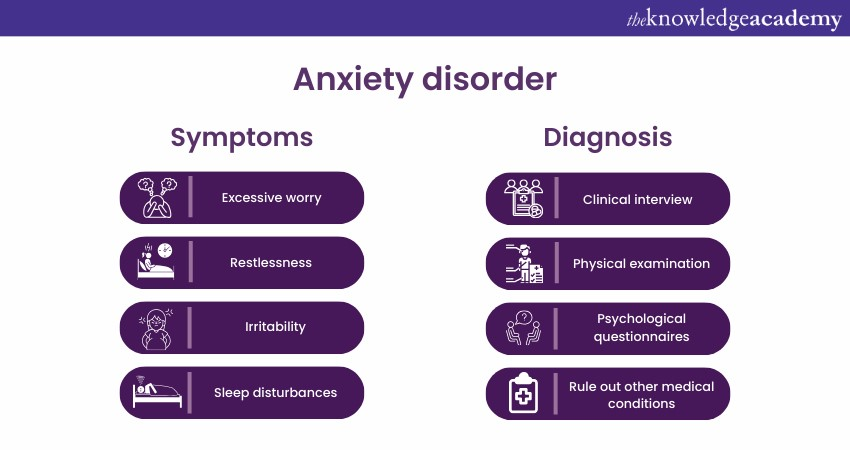
Anxiety disorders manifest with a range of physical and psychological symptoms. Commonly, individuals might experience restlessness, rapid heartbeat, trembling, muscle tension, sweating, and irritability. Chronic anxiety can also lead to gastrointestinal problems, frequent headaches, and insomnia.
For diagnosis of this mental disorder, doctors usually conduct a thorough clinical interview to understand the severity, duration, and nature of the symptoms. They may also use specific assessment tools or questionnaires to gauge the intensity of the anxiety.
4) Treatment and management
Thankfully, anxiety disorders are treatable, and many individuals find relief with appropriate intervention:
a) Psychotherapy: Cognitive-Behavioural Therapy (CBT) is particularly effective. It helps individuals recognise and challenge their patterns of thought and behaviour that contribute to anxiety.
b) Medication: Various classes, including Selective Serotonin Reuptake Inhibitors (SSRIs), benzodiazepines, and beta-blockers, can be prescribed based on the specific disorder and its severity.
c) Lifestyle changes: Regular exercise, meditation, deep breathing exercises, and being devoid of caffeine and certain medications can help manage symptoms.
Master your mind against anxiety with our Handle Anxiety Masterclass
Bipolar and related disorders
Bipolar and related disorders consist of a group of mood disorders that involve alternating episodes of depression and mania or hypomania. Characterised by extreme mood fluctuations, these disorders can significantly affect an individual's daily life, relationships, and overall well-being.
1) Nature and characteristics
Bipolar disorders are marked by significant shifts in mood, energy, and activity levels. Unlike the regular ups and downs everyone experiences, the mood episodes associated with bipolar disorders are more intense and can last for prolonged periods. Depending on the specific type, the intensity and duration of these episodes can vary.
2) Classification of bipolar disorders
a) Bipolar I disorder: This involves periods of severe mood episodes, transitioning from mania (or severe mood elevation) to depression. A manic episode may last for at least a week, often requiring immediate medical attention, while depressive episodes typically last two weeks or more.
b) Bipolar II disorder: Characterised by patterns of depressive episodes and hypomanic episodes (a milder form of mania that lasts for at least four days). However, it doesn’t have full-blown manic episodes like Bipolar I.
c) Cyclothymic disorder (Cyclothymia): A milder form of bipolar disorder, with periods of hypomanic symptoms and depressive symptoms that last for at least two years in adults or one year in children and adolescents.
3) Causes and risk factors
While the exact cause remains unknown, a combination of genetics, environment, and altered brain structure and chemistry may contribute.
a) Genetics: If an individual has a family history of bipolar disorder, it increases the risk.
b) Brain structure: Functional MRI and other imaging techniques indicate some differences in the brains of people with bipolar disorder.
c) Environmental factors: Trauma, extreme stress, physical illness, and other traumatic events might trigger or worsen symptoms.
d) Chemical imbalances: Neurotransmitter imbalances can play a crucial role.
4) Symptoms and diagnosis
While symptoms can differ based on the type of bipolar disorder, common episodes include:
a) Manic/hypomanic episodes: Elevated mood, increased energy, reduced need for sleep, fast speech, racing thoughts, increased self-esteem, distractibility, and more risk-taking behaviours.
b) Depressive episodes: Sadness, hopelessness, lethargy, insomnia or oversleeping, significant weight changes, feelings of worthlessness, inability to concentrate, and suicidal thoughts.
Diagnosing bipolar disorder involves a detailed clinical assessment, physical examination, psychiatric assessment, and mood charting to track mood fluctuations.
5) Treatment and Management
Managing bipolar disorder is a lifelong process and generally involves:
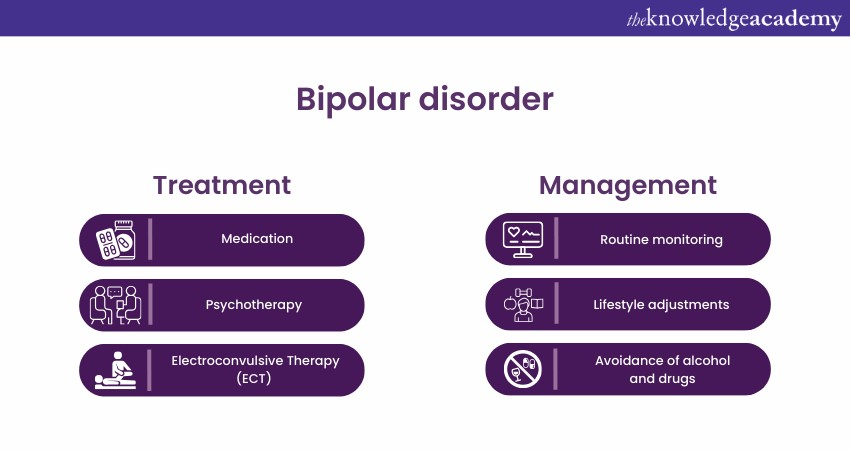
a) Medication: Mood stabilisers, antipsychotics, antidepressants, and anti-anxiety medications might be prescribed, depending on the specific symptoms.
b) Psychotherapy: Cognitive-Behavioural Therapy (CBT), family-focused therapy, and group therapy are effective in managing symptoms and triggers.
c) Lifestyle management: Regular sleep, a balanced diet, avoidance of alcohol and drugs, stress management, and routine monitoring are vital.
d) Electroconvulsive Therapy (ECT): In cases where medication and therapy aren’t effective, ECT might be considered.
6) Impact on daily life
Bipolar disorder can influence various life aspects, including relationships, jobs, and school performance, and even lead to substance abuse or legal issues. Effective management can minimise these impacts, helping individuals lead fulfilling lives.
Embrace the present and cultivate inner peace with our Mindfulness Training
Psychotic disorders
Psychotic disorders represent some of the most severe and disabling of Mental Health conditions. Characterised by a distorted sense of reality, they encompass a range of symptoms, including hallucinations, delusions, and disorganised thought patterns. These points will help you to understand more about this mental disorder:
1) Types of psychotic disorders
a) Schizophrenia: Perhaps the most recognised among psychotic disorders, schizophrenia is marked by a range of cognitive, behavioural, and emotional dysfunctions. It includes hallucinations, delusions, and severely disordered thinking and behaviour.
b) Schizoaffective disorder: This condition is a hybrid of schizophrenia and a mood disorder (either major depressive disorder or bipolar disorder). Individuals experience both psychotic symptoms and significant mood disruptions.
c) Brief psychotic disorder: As the name suggests, this condition is short-lived, typically arising suddenly in response to a significant stressor and resolving within a month.
d) Delusional disorder: This disorder is characterized predominantly by delusions — false, fixed beliefs that persist despite evidence to the contrary. These delusions are often plausible, unlike the bizarre delusions seen in schizophrenia.
e) Shared psychotic disorder (Folie à Deux): This rare condition involves delusions shared between two or more individuals who are closely related emotionally or by proximity.
2) Underlying causes
The exact origins of psychotic disorders remain a subject of intense research, but multiple factors contribute:
a) Biological: Abnormalities in brain structure or chemistry, particularly in neurotransmitters like dopamine, can predispose individuals to psychosis.
b) Genetics: If individuals have a family history of psychotic disorders, it increases one's susceptibility.
c) Environmental factors: Stressful life events, trauma, or substance abuse can act as triggers for the onset or exacerbation of psychotic symptoms.
d) Developmental factors: Prenatal exposure to certain infections or malnutrition, as well as complications during birth, can increase the chance of developing a psychotic disorder.
3) Symptoms and presentation
The hallmark features of psychotic disorders are:
a) Hallucinations: These are sensory experiences in the absence of an external stimulus. These can be auditory (hearing voices), visual, tactile, olfactory, or gustatory.
b) Delusions: Strongly held beliefs that are resistant to reasoning or contradictory evidence. They can be paranoid, grandiose, erotic, jealous, or somatic.
c) Disorganised thinking and speech: This might manifest as rapidly shifting topics or incoherent speech.
d) Negative symptoms: This includes emotional flatness, lack of motivation, and reduced social engagement.
4) Diagnosis and treatment
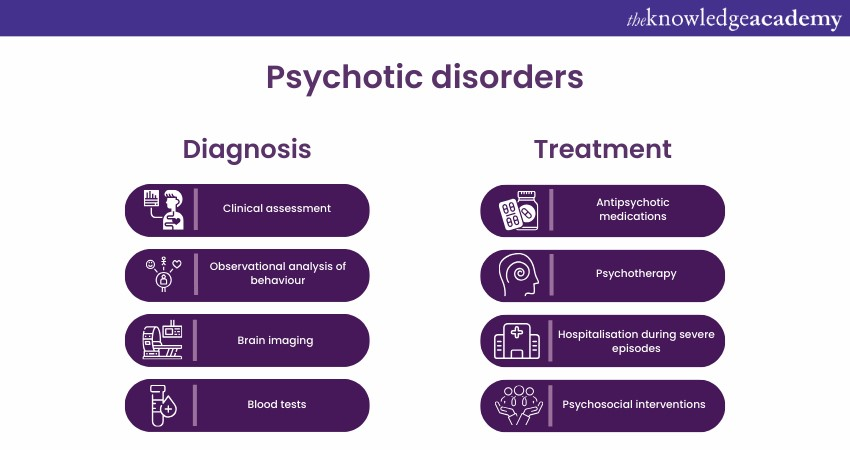
A thorough clinical assessment is crucial for diagnosis. This involves a comprehensive interview, medical examinations to rule out organic causes, and sometimes brain imaging. Once diagnosed, treatment typically involves:
a) Medication: Antipsychotics, such as risperidone, olanzapine, and clozapine, are primary in managing psychotic symptoms.
b) Psychotherapy: Cognitive-behavioural therapy can be adapted to help individuals recognise and challenge their delusions and hallucinations.
c) Supportive therapies: Social skills training, family therapy, and vocational rehabilitation can assist individuals in improving their daily functioning and interpersonal relationships.
Empower change and foster understanding – Register now in our Counselling Masterclass
Obsessive-compulsive and related disorders
Obsessive-compulsive and related disorders are conditions marked by patterns of persistent and intrusive thoughts (obsessions) and repetitive behaviours, mental acts (compulsions) that an individual feels driven to perform. These Psychological Disorders, deeply rooted in anxiety and distress, can dominate a person’s life, interfering with daily functioning and relationships.
1) Nature and characteristics
These mental disorders are mainly identified by obsessions and compulsions. Obsessions are unwelcome and distressing thoughts, images, or urges that repeatedly enter the mind. Compulsions can be characterised as repetitive behaviours or mental acts which are performed to reduce the distress or prevent a feared event. However, these compulsions offer only temporary relief and may not relate realistically to the obsessions.
2) Types of Obsessive-compulsive and related disorders

a) Obsessive-Compulsive Disorder (OCD): The most well-known of the group, OCD is characterised by persistent and unwanted obsessions, leading to engaging in compulsive behaviours. For example, an irrational fear of germs (obsession) might lead to excessive hand washing (compulsion).
b) Body Dysmorphic Disorder (BDD): People with BDD are excessively concerned about perceived flaws in their physical appearance, which to others are minor or not observable. They might repeatedly check their appearance or seek many cosmetic procedures.
c) Hoarding disorder: Individuals find it persistently difficult to part with possessions, regardless of their value, resulting in excessive accumulation and clutter, which can disrupt living spaces and overall life.
d) Trichotillomania (Hair-Pulling Disorder): This involves recurrent hair pulling, which results in noticeable hair loss and significant distress.
e) Excoriation (skin-picking) disorder: Characterised by repetitive skin picking, leading to skin lesions and attempts to stop the behaviour.
3) Causes and risk factors
a) Biological factors: Brain structure and functioning, along with neurotransmitter imbalances (especially serotonin), seem to play roles.
b) Genetics: Family studies suggest a genetic component, with some OCRDs running in families.
c) Environmental factors: Childhood trauma, infections, and significant life stressors might contribute.
d) Behavioural factors: Some theories suggest that compulsive behaviours arise from habits formed in response to situations.
4) Symptoms and diagnosis
Common symptoms of this mental disorder include:
a) For OCD: Unwanted forbidden or taboo thoughts involving harm, aggression, religion, or sexuality. Compulsions such as washing, checking, or mental acts like counting.
b) For BDD: Extreme focus on perceived physical flaws, leading to repetitive behaviours like mirror checking, grooming, or skin picking.
c) For hoarding: Inability to discard items, resulting in cluttered living areas.
Diagnosis involves comprehensive clinical interviews, symptom assessment scales, and ruling out other potential causes.
5) Treatment and management
a) Psychotherapy: Cognitive-Behavioural Therapy (CBT) is especially effective, focusing on exposure and response prevention to confront obsessions and reduce compulsive behaviours.
b) Medication: Selective Serotonin Reuptake Inhibitors (SSRIs) are prescribed for OCRDs, helping to reduce symptoms.
c) Deep Brain Stimulation (DBS): For severe cases, DBS can be considered, especially when standard treatments don’t provide relief.
6) Living with Obsessive- compulsive and related disorders
The impact of this mental disorder on daily life can be significant, affecting relationships, work, and general well-being. However, with timely intervention and support, many individuals can manage their symptoms and lead healthy lives.
Step forward in safeguarding mental well-being – Sign up for our Prevention Psychology Training
Conclusion
Understanding Psychological Disorders is crucial in today's world where Mental Health is gaining more recognition and emphasis. It's necessary that more education and awareness are required to spread its awareness. In this blog, you learnt about the different Psychological Disorders and how important it is to get the proper treatment to have good Mental Health.
Optimise workplace dynamics with our Psychology of Behaviour at Work Training
Frequently Asked Questions
Upcoming Health & Safety Resources Batches & Dates
Date
 Psychology Course
Psychology Course
Fri 14th Feb 2025
Fri 11th Apr 2025
Fri 13th Jun 2025
Fri 15th Aug 2025
Fri 10th Oct 2025
Fri 12th Dec 2025







 Top Rated Course
Top Rated Course



 If you wish to make any changes to your course, please
If you wish to make any changes to your course, please


